Cihan Atila, M.D., principal investigator Department of Endocrinology, Diabetology and Clinical Research, University Hospital Basel, University of Basel, Basel, Switzerland, reports that now, for the first time, researchers from the University of Basel and the University Hospital of Basel have succeeded in demonstrating a deficiency of oxytocin in patients with a deficiency of vasopressin (Arginine Vasopressin Deficiency, formerly central diabetes insipidus). This finding could be vital in developing new therapeutic approaches. The hormone oxytocin is essential for social interaction and to control emotions. A deficiency of this hormone has previously been assumed, for example, in people with autism, but it has never been proven.
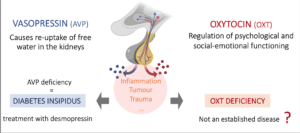 The hormones oxytocin and vasopressin are produced in the same area of the brain and are also very similar in structure. Patients with a rare vasopressin deficiency cannot concentrate their urine and lose liters of water as a result. In order to compensate for this loss, they are obliged to drink up to 10 liters or more per day.
The hormones oxytocin and vasopressin are produced in the same area of the brain and are also very similar in structure. Patients with a rare vasopressin deficiency cannot concentrate their urine and lose liters of water as a result. In order to compensate for this loss, they are obliged to drink up to 10 liters or more per day.
With a nasal spray or a tablet containing synthetically produced vasopressin (desmopressin), these symptoms can usually be treated without any problems. However, even with this treatment, many patients report anxiety, have trouble with social interactions, or demonstrate impaired emotional awareness.
These symptoms could be due to a deficiency of oxytocin, also known as the “bonding hormone.” “Because the production of the two hormones is so close anatomically, disorders that cause vasopressin deficiency could also affect the neurons that produce oxytocin,” explains Dr. Cihan Atila, endocrinologist and lead author of a study that has now been published in the journal Lancet Diabetes and Endocrinology.
Oxytocin boosters only work on the healthy.
Oxytocin is difficult to measure, and a “stimulation test” is needed to produce a reliable result. This test stimulates oxytocin secretion, i.e., the release of the hormone in the body. MDMA (3,4-methylenedioxy-N-methamphetamine), better known as ecstasy, is one such stimulant substance.
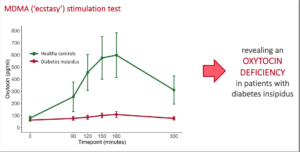 The researchers could show that oxytocin levels are 8.5 times higher in healthy individuals after a single dose of MDMA, while they remain unchanged in those with vasopressin deficiency (central diabetes insipidus). This provides strong evidence that their production of oxytocin is also impaired. As expected, the increase in oxytocin in healthy individuals after a dose of MDMA caused pro-social behavior and increased empathy, combined with a reduction in anxiety symptoms. The patients with vasopressin deficiency, on the other hand, showed no changes in these areas.
The researchers could show that oxytocin levels are 8.5 times higher in healthy individuals after a single dose of MDMA, while they remain unchanged in those with vasopressin deficiency (central diabetes insipidus). This provides strong evidence that their production of oxytocin is also impaired. As expected, the increase in oxytocin in healthy individuals after a dose of MDMA caused pro-social behavior and increased empathy, combined with a reduction in anxiety symptoms. The patients with vasopressin deficiency, on the other hand, showed no changes in these areas.
Therapy with oxytocin?
“These results, therefore, prove for the first time that a clinically relevant oxytocin deficiency actually exists. This finding opens up new therapeutic possibilities,” says Mirjam Christ-Crain, study leader and deputy head of endocrinology at the University Hospital.
In addition, the results contribute to a deeper understanding of oxytocin as a key hormone for socio-emotional effects. The same researchers at the Department of Clinical Research are currently planning a large study to investigate whether treatment with oxytocin can improve the psychological symptoms in patients with vasopressin deficiency.
Original publication:
Cihan Atila et al.
Oxytocin in response to MDMA provocation test in patients with arginine vasopressin deficiency (central diabetes insipidus): a single-center, case-control study with nested, randomized, double-blind, placebo-controlled crossover trial.
The Lancet Diabetes & Endocrinology (2023), doi: 10.1016/S2213-8587(23)00120-1
Read more about Dr. Atila’s breakthrough work in renaming Diabetes Insipidus to AVP Deficiency. This is the largest survey of patients with central diabetes insipidus, reporting a high prevalence of treatment-associated side effects, mismanagement during hospitalization, psychological comorbidities, and clear support for renaming the disease. Our data are the first to indicate the value of routinely omitting or delaying desmopressin.
For further contact: cihan.atila@usb.ch
© 2023, Pituitary World News. All rights reserved.
