From Lewis S Blevins, Jr MD – I spoke at a conference recently regarding testosterone replacement therapy in patients with male hypogonadism.
It was unusual conference populated by pharmacists, doctors of pharmacy, key decision makers for different insurance companies, other business people, physicians who are on the board of a company that decides whether to put different drugs on formulary, etc. One of the issues discussed was the controversial data regarding whether testosterone causes an increased number of cardiovascular deaths in men. There have been a couple of key studies, now considered to be flawed with calls for retraction, suggesting that men have a higher than expected mortality if treated with testosterone. In fact, the FDA recently reviewed about 5 such studies. Two showed a higher mortality, two showed improved mortality or, I should say, better survival, and one was inconclusive. Two different large meta-analyses, each including about 3000 patients were also reportedly reviewed. One of these showed increased mortality whereas the other one did not. Basically, when distilled down to the very nature of all of this, there is no real answer to this concern. Still, the FDA has required manufacturers of testosterone products to do studies to address this issue and also has added or recommended adding a black box warning on the labels or package inserts indicating that testosterone treatment may cause cardiovascular disease.
So, what is going on?
First, plenty of patients who have testosterone deficiency develop a syndrome called the metabolic syndrome and have increased cardiovascular risk as a result. Thus, some with profound and prolonged hypogonadism may be developing coronary disease during the time that they are not treated.
Second, being male, and having a typical male cholesterol profile, is more of a “risk factor” than being female and having estrogen sufficiency. By the way, after menopause, estrogen levels fall, the cholesterol profile changes, and then women ultimately “catch up” to men in their cardiovascular risk. At any rate, once the man starts testosterone his cholesterol profile becomes more male and that might be associated with a higher cardiovascular risk.
Third, many men with hypopituitarism have mild anemia due to testosterone deficiency. Other hormone deficiencies may contribute to the anemia. Taking testosterone can cause an increase in the number of red blood cells, and even frank polycythemia, which increases the viscosity of blood. Increased viscosity of the blood means it flows slower through blood vessels. If there is a narrowing in a blood vessel, such as in the coronary arteries, that slow flow might result in a small blood clot and lead to a heart attack. These observations and speculations make important to treat with testosterone in a way that does not elevate the hemoglobin and hematocrit levels.
So, what do I recommend?
I firmly believe in androgen replacement in men who have organic disease (hypothalamic or pituitary disease, testicular problems) causing their hypogonadism. Remember, hormone levels are low and we’re bringing them to normal. If this is done correctly, the risks should be no greater than simply being male.
It is essential to check levels and follow pharmacokinetics principles and dosage adjustments to ensure that the testosterone levels in response to treatment are”just right” implying not too low and not at all excessive.
I think it is wrong, because it is psychologically harmful, for the FDA and the other groups or societies to frighten otherwise healthy hypopituitary or hypogonadal men, many in their teens and also in the prime of their young adult lives, about the possible, but not proven, cardiovascular mortality of testosterone replacement.
I do, however, want to acknowledge that I believe that some patients with systemic illnesses, who develop secondary hypogonadism as a result, are likely to have complications of therapy. I like to think of the decline in testosterone (and growth hormone) levels in patients who are sick as perhaps protective adaptations to illness. It makes sense to shut down reproduction and growth when the organism has to divert energy to recovering from an illness or infection because reproduction and growth are functions that require a lot of energy. Thus, it may indeed be deleterious and not make sense to give testosterone to override the body’s normal mechanisms to compensate for illness. Some would argue that these compensatory mechanisms are examples of failed homeostasis. I can, on occasion, see their viewpoints but, on balance, believe that “Mother Nature” knows what she is doing. Thus, I am somewhat less interested in and less likely to recommend, treatment of those men who have systemic illnesses (liver disease, heart disease, diabetes, renal failure, Severe sleep apnea, chronic narcotic usage, polycythemia rubra vera, prostate cancer,etc) because I believe these patients to be at a higher risk for complications of testosterone treatment. Perhaps they are the ones who do have myocardial or other adverse events during treatment.
I am opposed to testosterone treatment for “symptomatic benefit” in men who do not have proven hypogonadism as evidenced by laboratory testing.
Testosterone is a “wonder drug” for those who truly have hypogonadism. Unfortunately, however, testosterone is a drug of misuse and abuse. Some patients try to “legitimize” the inappropriate use by going to physicians offices complaining of hypogonadal symptoms hoping for a prescription without so much as having levels checked. This is only to be regarded as an unconscionable practice of medicine as far as I am concerned. I believe, with the controversies surrounding the potential cardiovascular risks of therapy, the out-of-control direct consumer marketing, the marked increase in the number of prescriptions over the past decade, the costs of current therapies, and other factors that I won’t get into in this forum, will lead to a tightening of the prescribing practices of testosterone.
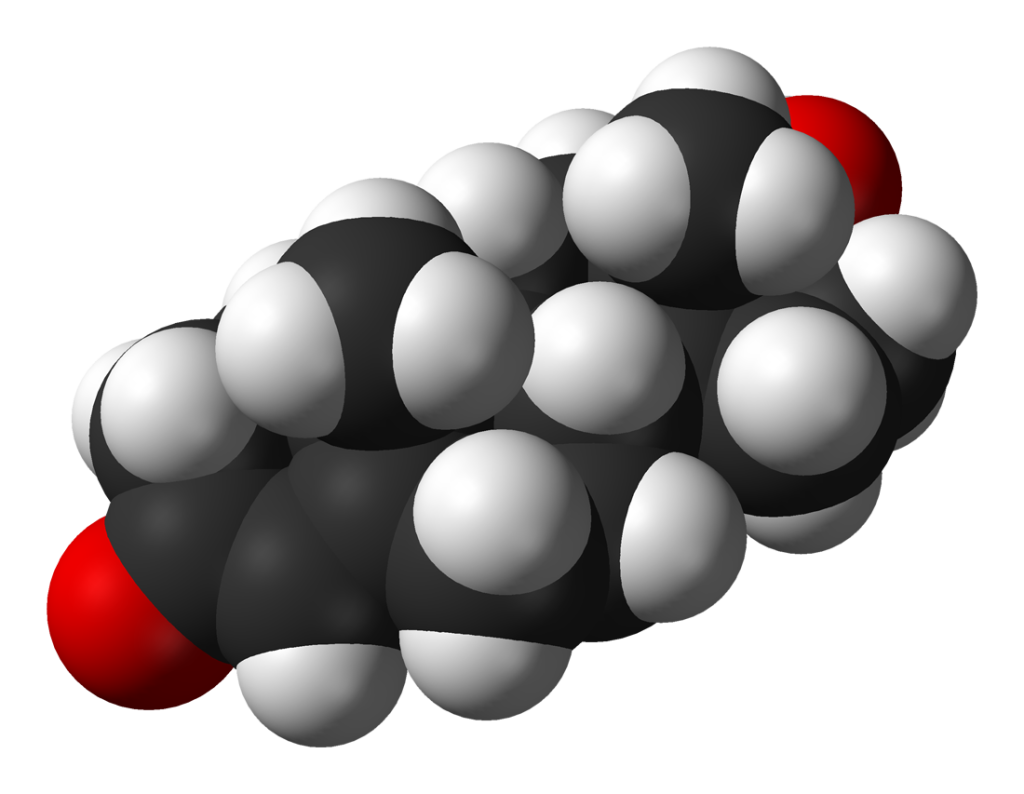
Graphic: “Testosterone-from-xtal-3D-vdW” by Ben Mills – Own work. Licensed under Public Domain via Wikimedia Commons
© 2015 – 2024, J D Faccinetti. All rights reserved.