A commentary from Dr. Lewis S Blevins Jr. co-founder – I was recently asked if I felt that we would ever be able to use stem cells to regenerate the pituitary gland.
Frankly, the answer is a resounding…..no.
There is no substitute for normal embryogenesis and embryology. The pituitary gland is a collection of cells that are grouped together to form the gland. There are, as most of you know, different cell types dispersed throughout the gland. Some of these cell types have their own particular locations where they are clustered. Each of the cell types occurs in different amounts based on evolutionary need as human beings. These cells indeed have come from stem cells. Different genes control their development and result in their individual identities. Between the cells is a remarkable delicate network of capillaries. There is an arterial supply, a venous supply, and venous drainage. More on this later to illustrate the complexity of the system. Furthermore, there are other cell types, elastin, reticulum, fibrocytes, collagen, etc that are interspersed between the cells and capillaries.
The bottom line, in any patient with pituitary disease, is that there has been a compromise in not only the cells but of all of these tissues that nature designed and grew to construct a pituitary gland. It is impossible to, in my mind at least, use stem cells, program them to turn on certain genes and turn off the others to differentiate into the different cell lines, learn them to secrete hormones, and populate the pituitary gland with the right amount of cells necessary to ultimately lead to normal pituitary and target gland function. Even if we could do that, I can’t imagine putting these highly differentiated cells in contact with the capillary network that would be necessary in order to ensure that the pituitary gland responds to brain and peripheral blood signals to coordinate hormone secretion to effectively control the relevant target glands.
Let’s focus on the blood supply of the pituitary gland and how important it is regarding function of the gland. Arterial blood supply, carrying oxygenated blood from the heart, is derived from the carotid artery through hypophyseal vessels to the pituitary gland. This blood carries hormones produced by the target gland and they are measured by the pituitary gland as other cells measure hormones, too.  Hormone binds to its receptor and activates things in the sale that goes to sell the information about how much of that hormone is present and then it regulates it’s hormone secretion. For example, if thyroid hormone levels are low the TSH producing cells of the pituitary will receive this blood, convert T4 to T3, T3 will then enter the cell nucleus and the amount of T3 will regulate TSH secretion, in this case the TSH-producing cell will recognize the T3 levels are low and make more TSH and release it in into the Capillaries near the sale which will carry it through venous channels that drain the pituitary from whence it is carried back to the heart, the blood is mixed, and the signal is sent to the thyroid. If the pituitary works and can secrete the TSH then the thyroid works more to bring up the T3 levels. The pituitary recognizes that and ratchets down the TSH. Interestingly, and perhaps unfortunately, the TSH producing cells can’t do this on their own. They have to have TRH from the brain to make a TSH molecule that works.
Hormone binds to its receptor and activates things in the sale that goes to sell the information about how much of that hormone is present and then it regulates it’s hormone secretion. For example, if thyroid hormone levels are low the TSH producing cells of the pituitary will receive this blood, convert T4 to T3, T3 will then enter the cell nucleus and the amount of T3 will regulate TSH secretion, in this case the TSH-producing cell will recognize the T3 levels are low and make more TSH and release it in into the Capillaries near the sale which will carry it through venous channels that drain the pituitary from whence it is carried back to the heart, the blood is mixed, and the signal is sent to the thyroid. If the pituitary works and can secrete the TSH then the thyroid works more to bring up the T3 levels. The pituitary recognizes that and ratchets down the TSH. Interestingly, and perhaps unfortunately, the TSH producing cells can’t do this on their own. They have to have TRH from the brain to make a TSH molecule that works.
There are blood vessels from the carotid artery that also supply the hypothalamus. They deliver T4 and T3 levels to hypothalamic cells that make TRH or thyrotropin releasing hormone. TRH is secreted into the capillaries within the hypothalamus. These capillaries then merge together to form when are called portal vessels. There are long and short portal vessels. Probably some medium ones, too. These portal vessels carry venous blood from the hypothalamus that contains the different releasing hormones for the different pituitary cell types. Once these portal vessels enter the anterior pituitary they break up into a network of small capillaries that merge with the capillaries from the arterial blood supply to the pituitary gland. The TRH from the hypothalamus gets delivered to the TSH-producing cells in this manner. This connection is vital. Again, if it doesn’t work, then the pituitary cell does not make a functional TSH molecule. And the thyroid doesn’t work. All of the different cell types in the pituitary gland have a hypothalamic influence and are dependent on this very unique portal system to function normally.
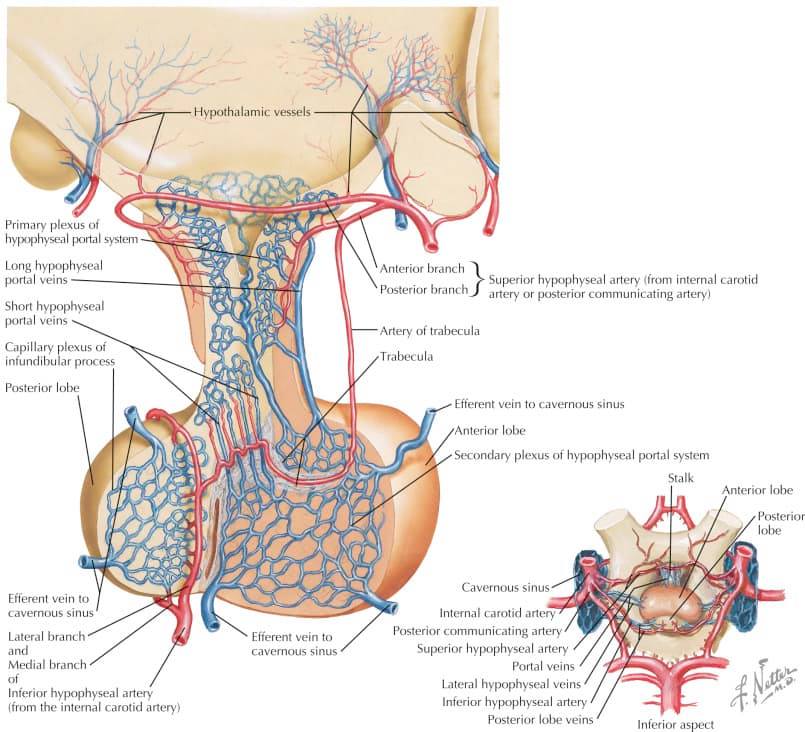 If this vascular system is disturbed in any way then the pituitary gland will not function and hypopituitarism will result. Unfortunately, this complex delicate and partially microscopic vascular system is often greatly disturbed by tumors, surgical intervention, head trauma, and other disease processes that affect the pituitary stalk and gland. When it is lost it doesn’t grow back. I don’t know of any way to cause it to regenerate and I can’t envision that we could ever reproduce this critical vascular system that would be required to make the pituitary gland function as intended even if we could differentiate pituitary cells, add them in proper amounts, and get them to stick together in some magical way.
If this vascular system is disturbed in any way then the pituitary gland will not function and hypopituitarism will result. Unfortunately, this complex delicate and partially microscopic vascular system is often greatly disturbed by tumors, surgical intervention, head trauma, and other disease processes that affect the pituitary stalk and gland. When it is lost it doesn’t grow back. I don’t know of any way to cause it to regenerate and I can’t envision that we could ever reproduce this critical vascular system that would be required to make the pituitary gland function as intended even if we could differentiate pituitary cells, add them in proper amounts, and get them to stick together in some magical way.
 Images that accompany these comments illustrate the artists renditions of the complexity of the vascular system of the hypothalamic-pituitary unit and also include some scanning electron micrograph views of the complex dense network of vessels and capillaries that ensure normal pituitary function. I find this system to be remarkably amazing. The truth is every part of us is equally complex and rather awe-inspiring.
Images that accompany these comments illustrate the artists renditions of the complexity of the vascular system of the hypothalamic-pituitary unit and also include some scanning electron micrograph views of the complex dense network of vessels and capillaries that ensure normal pituitary function. I find this system to be remarkably amazing. The truth is every part of us is equally complex and rather awe-inspiring.
© 2019 – 2024, Pituitary World News. All rights reserved.