From Lewis S Blevins Jr., MD – desamino d-arginine vasopressin…..in case you ever wondered.
DDAVP therapy has evolved somewhat over the past quarter of a century. When I started my training one of the common ways to administer DDAVP was in the form of Pitressin Tannate in oil. The injections were given intramuscularly as needed. Duration of effect was variable. I remember a few patients going several days before requiring subsequent injections. Most patients were satisfied with this form of therapy though it involved an intramuscular injection. In my experience, the risk of hyponatremia was higher then with more recent formulations of the drug.
DDAVP administered via the rhinal tube represented an advancement in drug delivery, permitted dose flexibility, and, though cumbersome, supplanted Pitressin Tannate injections. With this preparation, a small tube is attached to a bottle of DDAVP. They DDAVP is allowed to leak out into the tube, which is slightly bent, to measure out a dose of vasopressin. The tube permitted dose flexibility from, I believe, 2.5 µg to 10 µg of DDAVP. Once the tube was filled with the drug, patients carefully put one end of the tube in their nose, the other in their mouth, and blew the vasopressin into their nasal passages. Some patients blew to hard and ended up swallowing the drug rendering it ineffective. Others didn’t blow hard enough and the medication trickled out the nostril. With a little practice, patients could get it just right and have reliable delivery and subsequent absorption of the medication. I actually liked the dose flexibility offered by this preparation. The flexibility was far more important in children than it was in adults.
DDAVP nasal spray solution, perhaps the most commonly used product, delivers 10 µg of dDAVP per actuation. Thus, the dose is fixed. This preparation largely supplanted the rhinal tube. In my experience, the risk of hyponatremia is greater because in some patients one dose is not quite enough but two doses turns out to be excessive. I usually ask patients to use DDAVP when necessary. Most patients start by using one spray at bedtime. Bedtime dosing controls polyuria and allows for sleep. Some patients require an increase in the dose to two sprays at bedtime or one spray about every 12 hours as needed. The average patient requires 10 to 20 µg daily. Rarely, patients need 30 to 40 µg daily. I ask patients to have a period of time every day where they notice that their urine output picks up and they might even develop mild thirst. This allows for the release of excess amounts of water that might have been resorbed during the period of drug activity and protects against hyponatremia. Some patients notice that the nasal spray does not work as well if they have a cold and when pregnant. This is because the nasal passages produce an enzyme called vasopressinase that destroys vasopressin under certain circumstances.
DDAVP tablets are useful for those who prefer oral medications to nasal insufflated medications. Most of the DDAVP in the tablets is degraded by stomach acid. Thus, those who take antacids, drugs that inhibit gastric acid production, and the elderly who usually have lower amounts of stomach acid, require lower doses of the medication. Children require higher doses than do most adults. A typical starting dose would be 0.1–0.2 mg orally 2 to 3 times daily. Some children require up to 0.3 mg three times daily whereas elderly adults may require as little as 0.05 mg daily. Most importantly, patients should take as much as is needed. Some patients use the nasal spray on a daily basis and then use tablets for breakthrough polyuria during the day. Others use the nasal spray on a daily basis and revert to tablets during vacations because the nasal spray requires refrigeration whereas the tablets do not.
Some patients, and especially those who have undergone transphenoidal surgery, are unable to take vasopressin intranasally because of the surgery and packing materials that might prevent distribution of the drug across the nasal mucosa. Others may be critically ill and unable to take the medication via either the nasal or the oral routes for one reason or another. Fortunately, however, injectable vasopressin is available for use in the hospital. Aqueous vasopressin can be used in 3 to 5 unit dose strengths subcutaneously every 6 to 8 hours as needed to control polyuria. Alternatively, DDAVP may be administered subcutaneously by injection every 12 to 18 hours on an as needed basis. Since the medication is injected subcutaneously, and thus bypasses absorption via other routes, the doses used are much lower and average of 0.5–2 µg every 18 hours.
Here are some rough guesstimates, based on clinical experience, of dose equivalents that you can keep in mind, and keep handy, or share with your physicians should you be hospitalized for one reason or another and need to switch formulations to permit treatment in the hospital setting…….10 µg of intranasal DDAVP is equivalent to about 100 µg DDAVP administered twice-daily Orally, and about 0.5–1 µg DDAVP administered subcutaneously by injection every 18 hours. So, basically, because of the way vasopressin is formulated and administered, intranasal doses are about 10 times higher than the subcutaneous doses and oral doses are about 10 times higher than intranasal doses. That’s a hundred food spread from injected to orally administered dDDVP!
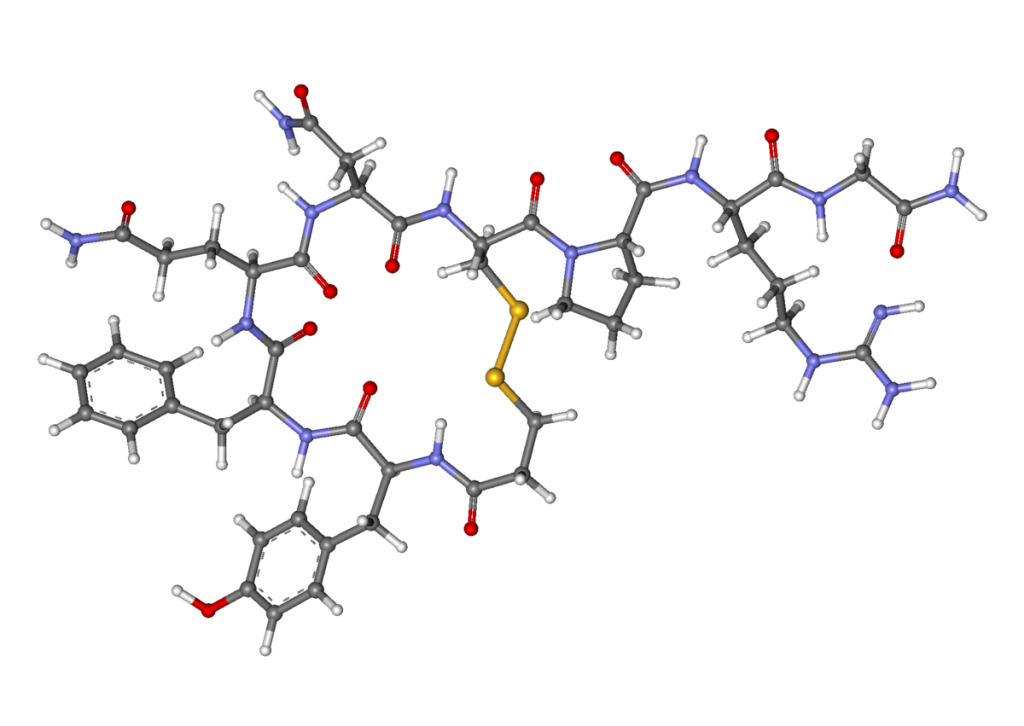
P.S, The d-arginine indicates it’s dextrorotatory instead of levorotatory…aaaaah….the days long ago of organic and biochemistry!
© 2014 – 2024, J D Faccinetti. All rights reserved.