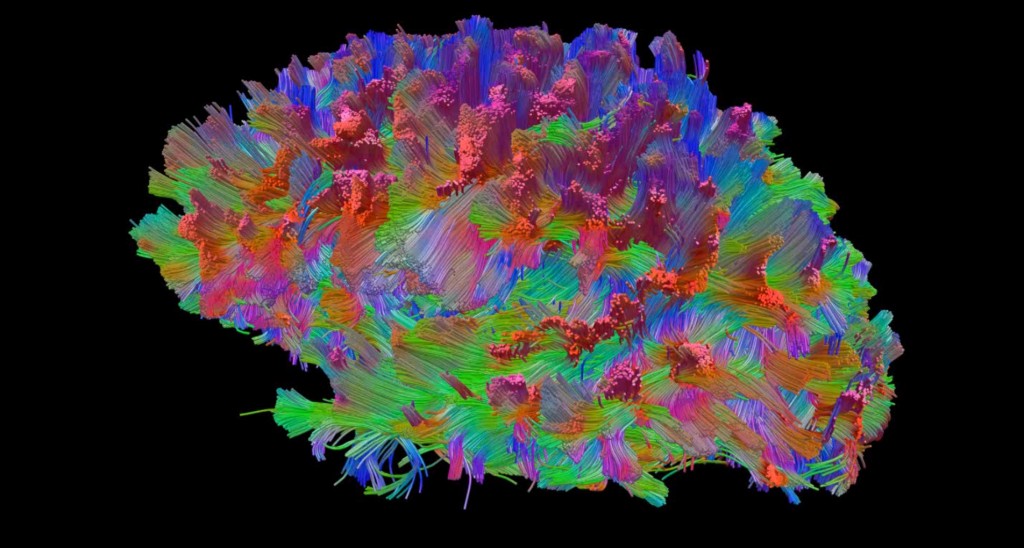
From Lewis Blevins, MD – Image from UPMC – The hypothalamus is recognized as the part of the brain that surrounds the third ventricle. It contains the cell bodies of neurons that release hypothalamic hormones that are transported to the anterior pituitary through the pituitary portal venous system to regulate pituitary function. It also contains the cell bodies of neurons that traverse the pituitary stalk and end up in the posterior pituitary and store vasopressin and oxytocin. The hypothalamus contains other cell bodies that do other things such as regulate the periodicity of certain hormonal systems. It has an area that senses thirst and changes in osmolarity. It regulates body temperature, appetite, feeding, and more. Several essential neurological pathways traverse the hypothalamus going from one place to another.
The hypothalamic hormones are released into the venous blood system of the hypothalamus which is drained by long veins, called portal veins, which go to the anterior pituitary. Once these hormones have their effect on pituitary cells, they are collected into the pituitary vein system and transported to the general circulation. Unfortunately, because of this design, the hypothalamic hormones, while they are in high concentration within the pituitary, are diluted rather quickly once they enter into the general circulation. Thus, hypothalamic hormones cannot be reliably measured in the general circulation because they are in such low concentration and, if they were measured, we could not gain any inferences about whether the amount of hormones directly affecting the pituitary gland was appropriate. So, we are left to draw inferences on hypothalamic function by an assessment of the functions of the pituitary gland and its target glands.
Hypothalamic dysfunction can lead to hypopituitarism. The pattern of laboratory abnormalities is similar to those seen in patients who have pituitary disorders. Hypothalamic disease is often associated with diabetes insipidus. Also, in the setting of otherwise normal pituitary function hypothalamic disease or interruption of the pituitary stalk may be associated with hypopituitarism, diabetes insipidus, and hyperprolactinemia. The hyperprolactinemia is because dopamine, produced by the hypothalamus, does not gain access to and suppress prolactin secretion by the pituitary gland. Thus, hyperprolactinemia in the setting of hypopituitarism and diabetes insipidus is often a sign of hypothalamic or pituitary stalk disease rather than pituitary disease. Rarely, patients with hypothalamic dysfunction have adipsic hypernatremia which is a condition where thirst is not sensed, water is not ingested, and then patient’s have dehydration with hypernatremia as a result. Some have coexisting mild diabetes insipidus.
There are a number of other conditions that result from hypothalamic dysfunction. For example, patients may have poikilothermia where their body temperature approaches that of the room temperature. They become febrile in hot environments and develop a low body temperature in cooler environments. In most cases, patients have a low body temperature or hypothermia. Patient’s may eat excessively, called hyperphagia, characterized by an insatiable desire to eat, and develop a morbid obesity. This is complicated by decreased autonomic outflow because of disruption of some of the autonomic pathways the pass thru the hypothalamus and a resulting lower metabolic rate. Excessive sleepiness, resulting in sleep up to 18 hours a day, is a rare problem while some children have persistent wakefulness.
Hypothalamic disorders or disease processes that can lead to hypothalamic dysfunction include: Craniopharyngioma, glioma, hamartoma, colloid cyst or ependymoma of the third ventricle, suprasellar Rathke’s cleft cyst, expansive chordoma, AV malformation, aneurysm and anterior communicating artery or other part of the circle of Willis, conventional radiotherapy for nasopharyngeal carcinoma or pituitary lesion, infiltrative disorders such as tuberculosis, sarcoidosis, Langerhans cell histiocytosis, head trauma, neurosurgical trauma, etc.
Hypopituitarism and diabetes insipidus are treated in the standard way. Patients with adipsic hypernatremia often require a water prescription. For example, a patient might be asked to drink 6-8 glasses of water daily depending on established needs. Drugs used experimentally to treat hypothalamic obesity include somatostatin analogs, hCG, and Dexedrine. Hypothermia is treated with passive warming and education so the patient’s know to avoid extremes of climate temperature.
© 2014 – 2024, J D Faccinetti. All rights reserved.